Translate this page into:
Preference of Tooth Extraction Over Root Canal Treatment among Patients Visiting Rural Health Centers—a Cross-Sectional Study
Address for correspondence Deesha Kumari, MDS, Department of Public Health Dentistry, AB Shetty Memorial Institute of Dental Sciences (ABSMIDS), Nitte (Deemed to be University), Mangalore 575018, Karnataka, India (e-mail: drdeesha.k@gmail.com).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background
Dental care decision-making is a multifaceted process influenced by various factors such as socioeconomic status, cultural beliefs, and access to healthcare resources. The research aims to elucidate the prevalence and determinants of the preference for tooth extraction over root canal treatment (RCT) in rural communities.
Methodology
A structured self-administered questionnaire comprising 15 close-ended questions was formulated for the purpose of data collection for this crosssectional survey and a sample size of 384 was estimated. Following a total enumeration sampling technique, the study was performed on individuals visiting the rural center aged over 18 years and persons who are willing to participate in the study. The data were analyzed using descriptive statistics and subjected to multinomial logistic regression.
Results
Among the participants, 33.1% had undergone RCT in the past and 63.5% had undergone extraction in the past with decay being the most common reason for seeking treatment. About 60.2% individuals preferred extraction and only 39.8% individuals preferred RCT wherein age, gender, and area of residence had a significant influence on the decision-making.
Conclusion
Majority of the participants in the study preferred extraction over RCT. Understanding the dynamics driving patient preferences in rural health settings is crucial for tailoring effective oral health interventions. The findings of this study have implications for healthcare practitioners, policymakers, and public health initiatives, providing valuable insights to enhance dental care delivery and promote informed decision-making in rural communities.
Keywords
root canal treatment
extraction
rural health centers
Introduction
Oral health is an integral component of overall well-being, yet the accessibility and utilization of dental care services remain disparate, especially in rural settings where unique challenges impede comprehensive healthcare delivery.1 One noteworthy aspect of oral health decision-making that has garnered attention is the distinct preference exhibited by patients in rural health centers when faced with the choice between treatment modalities. Rural-urban disparities in healthcare access have been well-documented, with rural populations often facing hurdles in receiving timely and appropriate dental care.2
In the context of this disparity, the prevalence of a particular preference for tooth extraction over root canal treatment (RCT) among patients in rural health centers raises intriguing questions. The inclination toward extraction might be influenced by various factors, such as economic considerations, cultural beliefs, and limited awareness about alternative treatment options.3 Socioeconomic factors significantly influence healthcare choices, and oral health is no exception. The economic considerations of patients in rural areas may lead them to favor tooth extraction as a seemingly more immediate and cost-effective solution compared with RCT.4 Additionally, the limited availability of dental care facilities in rural regions amplifies the impact of economic considerations, influencing patients to prioritize short-term solutions over the preservation of natural dentition. Cultural beliefs and perceptions surrounding dental procedures further contribute to the observed preferences in rural health centers. Deep-seated cultural norms and misconceptions may steer patients toward choices that align with their cultural expectations rather than evidence-based dental practices.5
Moreover, the inadequate awareness and education regarding the long-term benefits of RCT in rural areas exacerbate the preference for tooth extraction. The lack of information about alternative treatment options may lead patients to make decisions based on immediate relief and perceived affordability, without a comprehensive understanding of the potential consequences of choosing extraction over preservation.6 Examining the dynamics of patient choices in rural areas is pivotal to developing targeted interventions that not only bridge the existing gaps in oral healthcare but also cater to the specific needs and considerations of individuals residing in underserved rural communities. There is a limited amount of data available regarding the patient preference for teeth extraction over RCT among the Indian population. Therefore, this study aims to evaluate the patient's preference for tooth extraction over RCT.
Methodology
The study was performed at a rural satellite center affiliated with a tertiary dental school in South India. Ethical clearance for the study was obtained from the Institutional Ethics Committee (Ref. No. ETHICS/ABSMIDS/293/2022). A selfadministered questionnaire comprising 15 questions was formulated for the purpose of data collection for this cross-sectional survey. A total enumeration sampling method was followed. A proportion of 0.8, a precision of 5%, a desired confidence level of 95%, and a sample size of 384 were estimated. The study was performed on individuals over the age of 18 years and persons who are willing to participate in the study. Uncooperative patients as well as patients with functional disabilities were excluded.
Following an extensive literature review, an English draft of the questionnaire underwent evaluation for content and face validity by a panel of experts, using a 9-point criterion recommended by Oluwatayo.7 The questionnaire received a face validity score of 1.7 out of 3, indicating above-average validity. Subject matter experts assessed clarity, comprehensiveness, and appropriateness of the questionnaire's constructs, and an Aiken's V index score of 1.0 signified unanimous agreement among raters, confirming the instrument's reliability with a Cronbach's value of 0.8. Considering the rural satellite center's location where Kannada was predominantly spoken, the questionnaire underwent transliteration into Kannada. This translation process involved forward translation by the primary investigator and a Kannada professor, followed by a bilingual expert panel addressing inadequacies and discrepancies. The translated instrument was then back-translated into English by an independent translator, resulting in a refined Kannada version. The Kannada questionnaire underwent face and content validity assessment, following a similar process as the English version. Face validity scored 1.8 out of 3, and an Aiken's V index of 1.0 reiterated reliability with a Cronbach's value of 0.8. The questionnaire was made available to all the individuals visiting the rural dental satellite center. The questionnaire was divided into two parts. The first part comprised of demographic data and the second part explored about preference of tooth extraction over RCT among the individuals. No names were taken, hence ensuring anonymity of the responses.
The data were entered in Microsoft Excel and analyzed using SPSS version 23. The descriptive statistics are expressed in terms of number and percentage for ordinal and nominal variables, and continuous variables such as age are expressed as mean and standard deviation. Multinominal logistic regression was conducted to analyze the influence of various independent variables on the preference of treatment choice of individuals. A p-value of less than 0.05 was considered significant.
Results
A total number of 384 subjects responded to the questionnaire with a mean age of 41.47 ± 13.86. About 36.2% of the subjects belonged to the age group between 31 and 45 years, 27.3% belonged to the age group of 15 to 30 years, 24.5% belonged to the age group of 46 to 60 years, and 12% belonged to the age group of 61 to 75 years. Females accounted for 54.4% of the participants, while the males accounted for approximately 45.6%. Just over 78.9% of the participants were married, while remaining 21.1% of the participants were single. The greatest representation belonged to the upper lower (50.3), the lower (20.3), and the lower middle (15.9) socioeconomic status group, while the lowest representation came from the upper middle (13.5) socioeconomic status group.
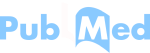
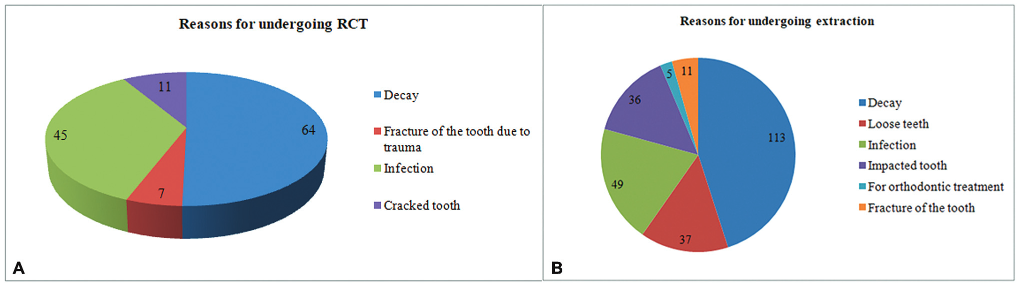
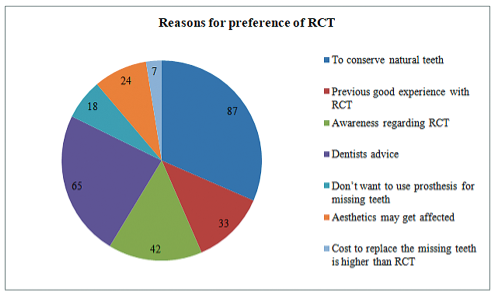
Among the participants, 127 (33.1%) had undergone RCT in the past and 240 (62.5%) had not undergone RCT in the past. Decays (50.4%) followed by infection (35.4%) were the most common reasons for undergoing RCT (Fig. 1A). Among the individuals who had undergone RCT in the past, 63.8% had experienced pain during the RCT or interappointment phase and 15.7% individuals had experienced pain in root canal-treated teeth after the RCT was completed (Table 1). Majority of the participants (51.2%) reported that the RCT procedure had scheduled two to three visits. Post-RCT, 60.6% participants had undergone postendodontic RCT restoration and crown placement (Table 1). A total of 244 (63.5%) individuals had undergone extraction in the past, whereas 32.8% individuals had not undergone extraction (Table 1). Decays (46.3%) followed by loose teeth (15.2%) were the most common reasons for undergoing extraction (Fig. 1B). On assessing the individual preferences of treatment choices between RCT and extraction, 60.2% individuals preferred extraction and only 39.8% individuals preferred RCT (Table 1 ). The most common reason given by individuals for preferring RCT was to conserve natural teeth (56.8%) followed by intention to follow dentist's advice (42.4%) and having awareness of RCT (27.4%) (Fig. 2). The most common reason given by individuals for preferring extraction was that they needed immediate relief from pain (78.7%), followed by the cost of RCT and crown (55.8%), the inconvenient appointment schedule for RCT (25.1%) and RCT being time-consuming in nature (24.2%) (Fig. 3).
- (A) Reasons of patients for undergoing RCT. (B) Reasons of patients for undergoing extraction.
- Reasons of patients for choosing RCT.
- Reasons of patients for choosing extraction.
| Questions | Frequency | Percent | |
|---|---|---|---|
| Undergone RCT in the past? | Yes | 127 | 33.1 |
| No | 240 | 62.5 | |
| Do not know | 17 | 4.4 | |
| Experienced pain during the RCT or interappointment phase? | Yes | 81 | 63.8 |
| No | 46 | 36.2 | |
| Experienced pain in root canal-treated after the RCT got completed? | Yes | 20 | 15.7 |
| No | 100 | 78.7 | |
| Do not know | 7 | 5.6 | |
| The number of visits required for RCT? | 1 visit | 8 | 6.3 |
| 2–3 visits | 65 | 51.2 | |
| >4 visits | 54 | 42.5 | |
| Got a postendodontic RCT restoration and crown placement done? | Yes | 77 | 60.6 |
| No | 43 | 33.8 | |
| Do not Know | 7 | 5.6 | |
| Undergone extraction of tooth in the past? | Yes | 244 | 63.5 |
| No | 126 | 32.8 | |
| Do not Know | 14 | 3.7 | |
| Preference: RCT or extraction? | Extraction | 231 | 60.2 |
| RCT | 153 | 39.8 | |
Abbreviation: RCT, root canal treatment.
The results from the final multivariate model are shown in Table 2. The effect of the independent variables such as age, gender, marital status, and place of residence on preference of individuals for RCT or extraction was analyzed. A 1 unit increase in age was associated with a 0.038 decrease in the relative log odds of choosing RCT over extraction. The relative log odds of choosing RCT over extraction would decrease by 0.496 in males as compared with females. In relation to the place of residence, individuals from the rural areas (odds ratio [OR] = 0.404, confidence interval [CI] = 0.204, 0.803) compared with individuals from urban and semi-urban areas were more likely to choose extraction over RCT. Socioeconomic status was not significant predictor of treatment choices.
| Variablesa | B | Std error | Sig | Exp(B) | 95% confidence interval for exp (B) | ||
|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||||
| Preference of RCT over extraction | Age | −0.038 | 0.009 | 0.000a | 0.963 | 0.945 | 0.980 |
| Male | −0.496 | 0.246 | 0.044a | 0.609 | 0.376 | 0.986 | |
| Married | −0.545 | 0.340 | 0.109 | 0.580 | 0.298 | 1.129 | |
| Urban | −0.769 | 0.481 | 0.109 | 0.463 | 0.181 | 1.189 | |
| Rural | −0.906 | 0.350 | 0.010a | 0.404 | 0.204 | 0.803 | |
| Upper middle | 0.685 | 0.446 | 0.125 | 1.984 | 0.828 | 4.753 | |
| Lower middle | 0.405 | 0.381 | 0.288 | 1.500 | 0.710 | 3.166 | |
| Upper lower | 0.564 | 0.302 | 0.062 | 1.758 | 0.972 | 3.177 | |
Abbreviation: RCT, root canal treatment.
Discussion
Root canal therapy and tooth extraction are among the most commonly administered treatments for pain relief. RCT aids in the retention of infected teeth that otherwise might have been extracted. Although RCT is highly prevalent, it is perceived by many patients as procedure to be feared. In the current study, 33.1% participants had undergone RCT with decay being the main reason to undergo RCT. A similar study by Bansal and Jain also reported a lower experience of RCT among individuals.5 On the contrary, a study by Pra-theebha et al reported that 80% patients had undergone RCT.6 These variations may be owed to various factors like oral health awareness and education levels within communities which significantly influence the demand for dental procedures such as RCTs. Regions with high dental health literacy may exhibit greater awareness of the importance of timely interventions, leading to higher rates of RCTs.8,9 About 63.8% patients experienced pain during RCT or interappointment phase. Similar results were found in a study by Iyer et al, wherein 66.67% patients with previous RCT reported having experienced pain at some point of RCT.10 RCT, in comparison to other dental procedures, tends to induce more frequent and severe postoperative pain, with reported frequencies ranging from 1.5 to 53%. Notably, over 50% of patients undergoing RCT experience intense postoperative pain. The origins of this pain are diverse, potentially stemming from mechanical, chemical, and/or microbial injuries to dental tissues during or aggravated by RCT. Additionally, psychological factors such as the fear of dental treatment and anxiety have been recognized for their influence on pain perception.10,11
The present study showed that majority of the patients had completed their RCT in two to three visits, while 42.5% patients had more than four visits for their treatment. The advent of advanced automated tools in the field of endodon-tics has made it feasible to perform RCT in a single visit. A growing number of dentists are adopting single-visit end-odontics as a central element of contemporary practice. Conversely, some practitioners adhere to the traditional multiple-visit protocol, emphasizing its extensive history and high clinical success rate. Literature indicates that a majority of practitioners (52.4%) complete RCTs in three visits, with 26.8% opting for a single-sitting approach, while a minimal percentage of dentists choose to complete RCT in more than three visits.12
On assessing the individual preferences of treatment choices between RCT and extraction, 60.2% individuals preferred extraction and only 39.8% individuals preferred RCT in the present study. The intention to conserve natural teeth was the major factor for patients preferring RCT. On the contrary, immediate relief from pain was the driving factor for patients opting for extraction. These results were similar to a study by Sadasiva et al, wherein early 13.19% of the patients who participated in the survey were not worried about tooth loss and required immediate pain relief. About 3.03% of the patients opted out of RCT, as they feel that they cannot come for multiple visits and prolonged treatment periods since they are old.4 The present study determined that age, gender, and place of residence were associated with individual's choices of treatment preferences. A study by Gbadebo and Adebayo showed that affordability of treatment, fear of drilling, and fear of injection were associated with the choice of patient's not to opt for RCT.13
However, the study has certain limitations. First, the cross-sectional design restricts our ability to establish causality between patient preferences and various factors, as it only provides a snapshot of preferences at a specific point in time. Longitudinal studies could offer a more comprehensive understanding of how preferences evolve over time and the factors influencing these changes. Second, the reliance on self-reported data introduces the possibility of recall bias, as patients may not accurately recall or disclose their preferences due to social desirability or other cognitive biases. Additionally, the study's focus on rural health centers may limit the generalizability of findings to urban or suburban populations, warranting caution in extrapolating these results to different healthcare settings.
Despite its limitations, this study opens avenues for future research in the realm of patient preferences for dental procedures in rural health settings. Future studies could employ qualitative research methods, such as interviews or focus group discussions, to delve deeper into the underlying reasons behind patient preferences. Understanding the cultural, socioeconomic, and educational factors that influence these preferences could provide valuable insights for healthcare practitioners and policymakers aiming to improve oral health outcomes in rural areas. Furthermore, longitudinal studies tracking changes in preferences over time and in response to interventions could offer a more dynamic perspective on patient decision-making. Exploring the impact of oral health education programs on patient awareness and preferences may also be a fruitful avenue for future research, contributing to the development of targeted interventions aimed at promoting evidence-based decisionmaking in dental care.14,15 Qualitative studies involving healthcare providers may offer insights into the challenges faced in communicating the benefits of RCT versus tooth extraction, informing the development of effective patient education strategies. Furthermore, interdisciplinary research could explore the role of cultural perceptions, social norms, and economic factors in shaping patient preferences, paving the way for holistic interventions that address the root causes of these preferences rather than merely their symptoms.
The findings of this study, while limited in scope, carry important implications for oral health policy in rural areas. Future research should explore how policy interventions, such as incentivizing rural dentists to provide RCTs or enhancing the accessibility of endodontic services, may impact patient preferences. Policymakers can benefit from a nuanced understanding of the factors influencing patient choices to develop targeted strategies that align with the preferences and needs of rural populations. Moreover, the study calls for a broader discourse on oral health policies that recognize the unique challenges faced by rural communities and seek to address disparities in access to comprehensive dental care.
Conclusion
This cross-sectional study on the preference of tooth extraction over RCT among patients visiting rural health centers sheds light on a significant aspect of oral healthcare decisionmaking in underserved communities. The findings underscore the prevalent inclination toward tooth extraction among the rural patient population, emphasizing the need for a nuanced understanding of the factors influencing such preferences. By fostering a patient-centered approach and aligning healthcare services with the preferences and needs of the population, it is possible to advance oral health outcomes and contribute to the development of equitable and effective oral healthcare strategies in rural health settings.
Authors' Contributions
S.S., D.K., S.B., and S.A.A.G.A. all played significant roles in the conceptualization of the topic, conducting literature searches, collecting data, and writing and finalizing the manuscript. D.K. specifically contributed to the data analysis in addition to these tasks.
Conflict of Interest
None declared.
References
- Prevalence of toothache and associated factors: a population-based study in southeast iran. Iran Endod J. 2013;8(03):123-128.
- [Google Scholar]
- Disparities in access to oral health care. Annu Rev Public Health. 2020;41:513-535.
- [Google Scholar]
- Survey-based research on patients' knowledge about endodontic treatment. Zdrow Publiczne. 2014;124:134-137.
- [Google Scholar]
- Analyzing the reasons for patients opting-out from root canal treatment and preferring extraction in south Indian population prospective study. Int J Prosthodont Restor Dent. 2018;8(04):108-113.
- [Google Scholar]
- An insight into patient's perceptions regarding root canal treatment: A questionnaire-based survey. J Family Med Prim Care. 2020;9(02):1020-1027.
- [Google Scholar]
- Knowledge, awareness, and perception on root canal treatment among South Indian population A survey. J Adv Pharm Technol Res. 2022;13(Suppl 1):S302-S307.
- [Google Scholar]
- Validity and reliability issues in educational research. J Educ Soc Res. 2012;2(02):391.
- [Google Scholar]
- Non-clinical influences on clinical decision-making: a major challenge to evidence-based practice. J R Soc Med. 2010;103(05):178-187.
- [Google Scholar]
- Awareness of the causes and management of endodontic mishaps among dental students at King Saud University and Riyadh Al-Elm: a cross-sectional study. J Nat Sci Med. 2023;6:38-45.
- [Google Scholar]
- Dental patient's knowledge, awareness and attitude towards root canal treatment: a survey based research. Int J Recent Sci Res. 2018;9(01):23214-23218.
- [Google Scholar]
- Pain prevalence and severity before, during, and after root canal treatment: a systematic review. J Endod. 2011;37(04):429-438.
- [Google Scholar]
- Attitude of general dental practitioners toward root canal treatment procedures in India. J Contemp Dent Pract. 2013;14(03):528-531.
- [Google Scholar]
- Factors associated with patients' rejection of root canal treatment in a tertiary hospital, southwest Nigeria: a pilot survey. J West Afr Coll Surg. 2023;13(03):22-27.
- [Google Scholar]
- Root canal treatment in elderly patients: a review and clinical considerations. Saudi Med J. 2019;40(03):217-223.
- [Google Scholar]
- Retrospective cross sectional comparison of initial nonsurgical endodontic treatment and single-tooth implants. Compend Contin Educ Dent. 2007;28(06):296-301.
- [Google Scholar]