Translate this page into:
Forgotten and Found: Neglected Omphalocele - Vital Role of Imaging
Address for correspondence Neha Bagri, MD Radio-diagnosis, Associate Professor, Department of Radio-diagnosis, VMMC & Safdarjung Hospital, New Delhi 110029, India (e-mail: drnehabagri@gmail.com).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background
Omphalocele is a congenital abnormality of the abdominal wall consisting of protrusion of the abdominal contents at the base of the umbilical cord. It is associated with genetic and structural defects, which significantly affect its prognosis and survival outcomes.
Case Presentation
Prenatal diagnosis of this condition is crucial for apt management; however, we present two cases of neglected and giant omphaloceles in early childhood. It is usually a disease of neonatal age, and presentation at such a late age is quite rare. The management of such cases is quite challenging, and multiple strategies have been described. In our case, the giant omphalocele was managed with an external surgical skin closure system as a component of a staged closure strategy. Conclusion The expert surgical technique played a decisive role, allowing the coordination of a multidisciplinary team, which was crucial for optimal management.
Keywords
omphalocele
congenital
neglected
giant
Background
Omphalocele is a congenital malformation of the abdominal wall in which the contents protrude into a thin-walled sac outside the abdominal cavity. Herniation usually occurs at the base of the umbilical cord and involves the intestines and liver.1 The estimated prevalence of omphalocele is approximately 1 in every 3,000 to 10,000 live births.2 Most of these defects can be diagnosed on antenatal screening tests, and the prognosis depends upon the sac's contents, the defect's size, and other associated anomalies.3
The definition of giant omphalocele includes a defect that contains more than 75% or larger than 5 cm liver within the sac.2 Giant omphalocele constitutes a significant subgroup among infants with omphalocele. While primary closure of the fascial defect can be performed in cases of small omphaloceles, management becomes more intricate in giant omphaloceles.2 It is frequently accompanied by various other congenital anomalies and long-term complications, leading to a worse prognosis. On the contrary, small omphaloceles typically have a favorable prognosis, especially when there are no associated life-threatening congenital malformations or syndromes.4
Here, we present three rare cases of giant neglected omphaloceles in toddler age groups with large bulging abdominal masses and associated multiple congenital anomalies, calling attention to imaging in these cases.
Case 1
This report presents an unusual case of giant omphalocele in middle childhood. Typically diagnosed antenatally through routine prenatal screening, omphaloceles are comparatively rare in postnatal settings.
We present the case of a 7-year-old boy who presented to our hospital with complaints of abdominal swelling since birth. The child was born full-term via normal vaginal delivery at home and cried immediately after birth. Per abdomen examination, a large anterior abdominal wall defect of approximately 6 × 8 cm was seen with an overlying expansile swelling of about 10 × 10 cm, showing positive cough impulse (expansion upon coughing; Fig.l). A clinical diagnosis of epigastric omphalocele was made, and the child was referred to the department of radiodiagnosis for imaging and further workup.

- (a, b) Clinical picture (frontal and lateral view) of the child showing a large expansile abdominal swelling.
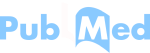
Ultrasonography (USG) evaluation was performed on a Philips Affiniti 70 machine, which showed herniation of the right lobe of the liver with the portal vein and hepatic veins into the sac. The left lobe of the liver was visualized at the standard anatomical location. The spleen appeared distorted in shape with posterior hilum but appeared in the standard anatomical location. A few bowel loops were also noted in the herniated sac (Fig. 2).
- (a, b) Ultrasonography (USG) of the abdomen showing herniation of the right lobe of the liver with portal and hepatic veins into the sac. (c) Distorted spleen, but with normal anatomical location. (d) Few bowel loops in the herniated sac.
Two-dimensional (2D) echocardiography was performed for the patient to rule out any associated congenital abnormalities. It revealed situs solitus with levocardia and normal atrioventricular (AV) and ventriculoarterial (VA) concordance. Inferior and superior venae cavae were seen draining generally into the right atria, with four pulmonary veins draining into the left atria. The biventricular function was normal with a conventional left-sided aortic arch. There was no evidence of atrial/ventricular septal defect, patent ductus arteriosus, or coarctation of the aorta.
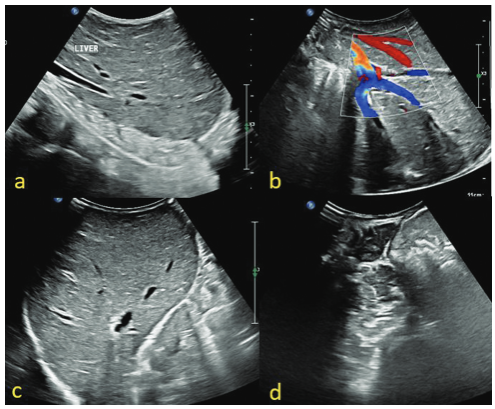
A contrast-enhanced computed tomography (CECT) scan of the abdomen was then performed at our department for presurgical planning on a 256-slice dual-source CT scanner, which demonstrated a significant anterior abdominal wall defect with loss of domain hernia (TANAKA's index 0.71). There was herniation of the liver, gall bladder, portal vein common bile duct, and part of the stomach and bowel loops through the defect ( Fig. 3 ). The body of the pancreas appeared convex and pulled anteriorly in the abdominal cavity; however, it was normal in anatomical location and attenuation. The spleen and bilateral kidneys with adrenals were normal in morphology, attenuation, and enhancement. This comprehensive imaging study aided subsequent surgical decisions and management strategies for this intricate case.

- (a-c) Contrast-enhanced computed tomography (CECT) images showing herniation of the liver, gall bladder, portal vein and common bile duct, part of the stomach, and bowel loops through the defect. (d) Volume-rendered three-dimensional (3D) image showing a large omphalocele.
Case 2
In the second case, we present another case of neglected omphalocele with various other associated malformations. An 8-year-old boy presented to our hospital with complaints of significant abdominal swelling that has been progressively increasing since birth. The patient was referred to the department of radiodiagnosis for imaging and further workup.
USG showed herniation of the left lobe of the liver with portal venules and bile ductules into the sac. The spleen was lying in the pelvis in the midline with a mildly distorted shape. CECT of the chest and abdomen were performed to further evaluate any other anatomical variants or abnormalities.
CECT of the chest revealed situs solitus with levocardia and a normal four-chamber heart. The trachea was midline with normal position, caliber, and course of significant bronchi. CECT of the abdomen demonstrated a single, substantial, anterior abdominal wall defect of size 10.7 × 11.3 cm (anteroposterior [AP] × craniocaudal [CC]) with herniation of the left lobe of the liver along with its portal venules and bile ductules (TANAKA index: 0.16; with no signs of loss of domain). A well-distended gall bladder was lying in the midline. The spleen (9.1 cm) was lying in the left lumbar region (lower border of L2-S1 vertebrae), showing only minimal capsular enhancement. A few branches of the splenic vein were seen along its capsule, draining into the main splenic veins. A hypertrophied splenunculus was seen at the superior border measuring approximately 29 × 16 mm, with its vein (6 mm) draining into the superior mesenteric vein (SMV) to form the portal vein (11 mm). The left portal vein branch was pulled outside, in the herniated sac, suggestive of wandering infarcted spleen (Fig. 4). The inferior mesenteric vein appeared prominent with ordinary course and termination. The superior mesenteric artery (SMA) and celiac arteries arose from the common trunk at the T12 vertebral level. The SMV and SMA relation was also reversed. The duodenum was not crossing the midline, and the duodenojejunal flexure was lying on the right side of the vertebrae. The suprahepatic inferior vena cava (IVC) and middle hepatic vein were mildly prominent (23 and 11mm, respectively). The bilateral kidneys were lying in the subdiaphragmatic location and were unremarkable. The spinous process of L5 and S1 were unfused without meningeal herniation–spina bifida occulta.
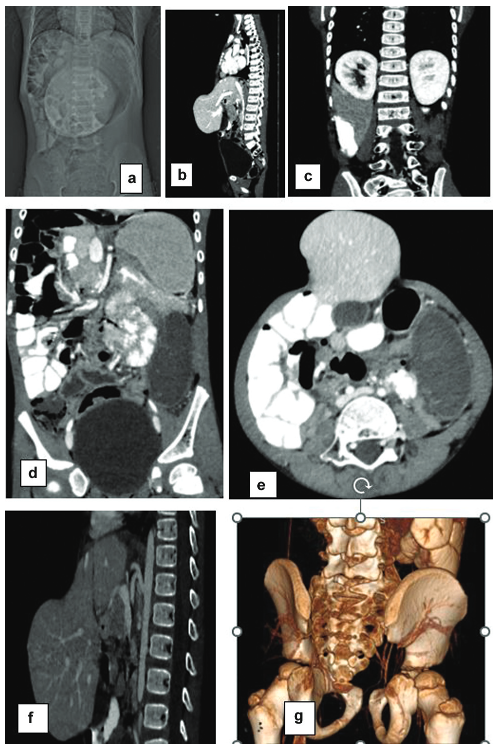
- (a) X-ray showing midline intra-abdominal well-defined round opacity. (b) Computed tomography (CT) images showing a large, anterior abdominal wall defect with herniation of the liver with midline gall bladder. (c) Bilateral kidneys were lying at the subdiaphragmatic location. (d, e) Infarcted wandering spleen with hypertrophied splenunculus. (f) Common origin of the superior mesenteric artery (SMA) and celiac trunk. (g) Spina bifida.
This detailed imaging study helped in surgical decisions and management of this peculiar case, thus highlighting the crucial role of cross-sectional imaging in neglected omphaloceles with delayed presentation.
Case 3
In another similar case, a 5-month-old infant presented with a bulging abdominal mass and was suspected to have an omphalocele upon clinical examination. The patient was referred to the department of radiodiagnosis for imaging. Ultrasound was performed, followed by a CT scan, which revealed a significant abdominal wall defect with herniation of the liver, gall bladder, portal vein, common bile duct, part of stomach, pancreas, and bowel loops (Fig. 5). Remarkably, this postnatal diagnosis defies the norm of antenatal detection. Despite the diagnosis, the patient was unfortunately lost to follow-up, underlining a critical challenge in the continuity of care.
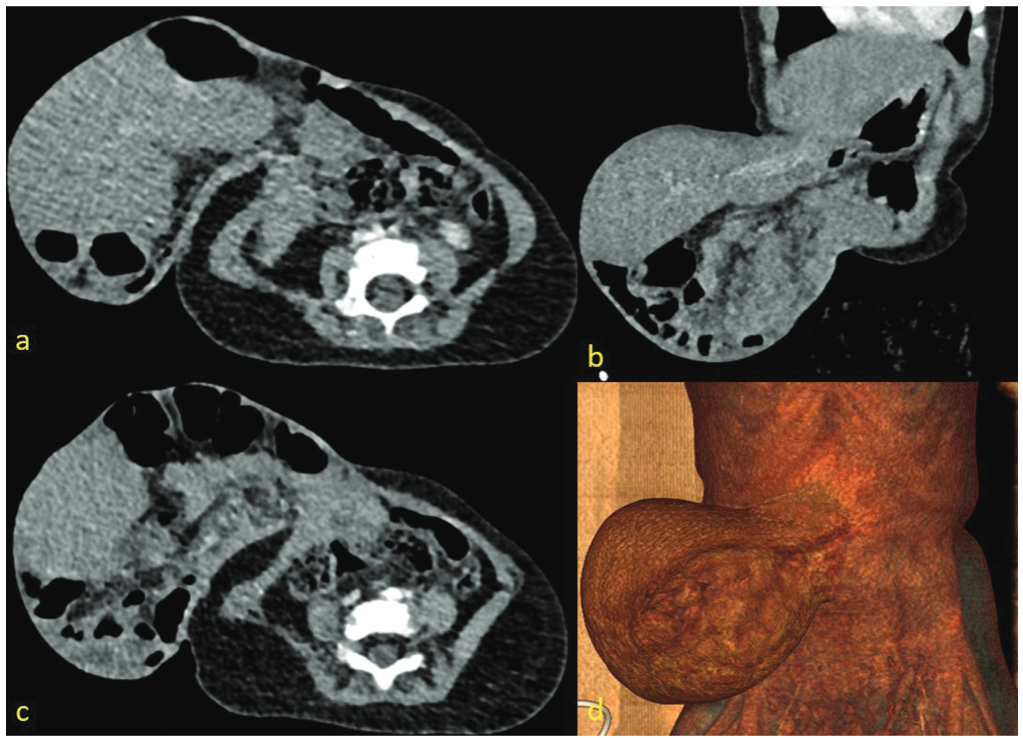
- (a-c) Contrast-enhanced computed tomography (CECT) scan of 5-month-old child showing a large abdominal wall defect with herniation of the liver, gall bladder, common bile duct, portal vein, part of stomach, pancreas, and bowel loops. (d) Volume-rendered three-dimensional (3D) image showing a large omphalocele.
Discussion
Giant omphaloceles are a remarkable rarity in pediatric patients, presenting clinicians with a complex puzzle. They demand a multidisciplinary approach for optimal management. In addressing the unique challenges posed by the substantial omphalocele in our first case, an innovative technique was employed to optimize outcomes. The indigenous portion of the hernial sac was expertly repurposed to serve as a protective layer for the exposed bowel and liver surfaces. This strategic approach aimed to prevent direct adhesion between the mesh and the delicate organs, a potential concern in such cases. Over this indigenous sac covering, mesh was placed, which is essentially used to reduce bleeding from minor surfaces of solid organs. A mixed mesh comprising of Prolene and Monocryl was then placed over it. To finalize the procedure, meticulously fashioned skin flaps were utilized to enclose the layers mentioned above, ensuring thorough coverage.
Given the size of the defect in the first case, mitigating the risk of abdominal compartment syndrome was paramount. The inherent challenge lies in devising surgical interventions suitable for a young child. There were only two viable surgical approaches in our case: one involving the placement of a temporary silo to gradually accommodate the abdominal contents and the other, the chosen method, akin to component separation and primary repair. Since the rectus muscle was significantly splayed apart, releasing incisions were skillfully executed along the lateral aspect of the rectus abdominis. In this approach, portions of the hernial sac were intentionally left adherent to the rectus muscle bilaterally, while the intermediate portion of the sac was excised ( Fig. 6). This novel modification facilitated the use of the sac as a protective barrier for the liver and bowel and leveraged the sac's natural thickening over time. This creative surgical technique addressed the immediate anatomical complexities and considered the patient s developmental nuances, underscoring the importance of tailored approaches in such intricate cases. Notably, the surgical intervention proceeded without complications, reflecting a smooth course. At present, the child is doing well and is in a favorable state of health, a testament to the success of the management approach.
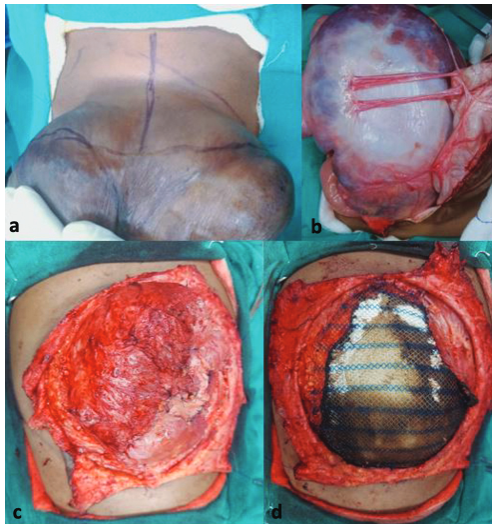
- (a-d) Postsurgical pictures of case 1 showing portions of the hernial sac left adherent to the rectus muscle bilaterally, with excision of the intermediate portion.
The cases presented here stand out not only due to the sheer uniqueness of such extensive omphaloceles in children but also because of the importance of imaging, the need to look for other associated anomalies, and the ingenious and unprecedented approach adopted for management. In the first case, the employment of the hernial sac itself as a protective barrier, coupled with meticulous surgical execution, highlights the potential of innovative strategies in addressing challenging cases within this limited domain.
Conclusion
The triumphant management of these cases underscores the indispensability of a multidisciplinary approach. Integrating innovative surgical strategies with a diverse range of diagnostic medical insights can meticulously manage such intricate pediatric congenital anomalies.
Acknowledgments
We wish to thank the staff at the Department of Radiodiagnosis, VMMC and Safdarjung Hospital, for their support and cooperation throughout the study. All the patients are acknowledged for participation in this research.
Ethical Approval and Consent to Participate
A written informed consent was obtained from the participants.
Availability of Data and Materials
The cases and the images are available from the Department of Radiodiagnosis, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India.
Authors' Contributions
N.B. is the corresponding author, designed and revised the work, interpreted the data, submitted the case, drafted the work, and approved the submitted version for publication. R.M. contributed to revision of the manuscript and approved the submitted version for publication. R.M. and P.M. contributed to revision of the work. J.G. provided the subjects for the study. All authors read and approved the final manuscript.
Conflict of Interest
None declared.
References
- Giant isolated omphalocele: role of prenatal diagnosis in prognostic assessment and perinatal management. Case Rep Med. 2020;2020:4578912.
- [Google Scholar]
- Outcomes in the giant omphalocele population: a single center comprehensive experience. J Pediatr Surg. 2020;55(09):1866-1871.
- [Google Scholar]
- Giant Omphalocele with skeletal deformities: a case report. Int J Contemp Pediatr. 2018;5(03):1142.
- [Google Scholar]
- Long term complications and outcomes in omphalocele. Semin Pediatr Surg. 2019;28(02):118-121.
- [Google Scholar]