Translate this page into:
Knowledge and Awareness of Pelvic Floor Disorders and Rehabilitation in Postpartum Women: An Observational Study
Address for correspondence Zankhana Parikh, Department of OBG Physiotherapy, Institute of Physiotherapy, KLE Academy of Higher education and Research, Belagavi, Karnataka 590010, India (e-mail: zankhana.parikh21@gmail.com).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background
The prevalence of pelvic floor disorders (PFDs) is considerably high, yet, only a handful of women seek help as most of them accept it as a consequence of pregnancy, childbirth, and as a part of aging process. Pelvic floor physiotherapy is considered primary treatment for management of PFDs. Inadequate knowledge is a major obstacle in seeking appropriate treatment. The present study intends to evaluate the knowledge and awareness of PFDs and rehabilitation in postpartum women.
Methodology
The study comprised of 316 postpartum women from a tertiary care center in Belagavi district. Data was collected through an interviewer-administered questionnaire about PFDs and questions to assess awareness of pelvic floor physiotherapy. Outcome Measures Australian Pelvic Floor Questionnaire which comprises of 42 questions, divided in 4 domains, about bladder, bowel, prolapse, and sexual function was used along with 6 self-designed questions about pelvic floor physiotherapy, to evaluate the knowledge of PFDs and rehabilitation.
Results
The statistical analysis was done using the SPSS software version 26. The prevalence of PFDs was 63.6% with bladder component affected in 54.11%, bowel in 26.8%, prolapse symptoms in 2.21%, and sexual function in 22% postpartum women. They lacked knowledge regarding PFDs and rehabilitation with 84.4% considering the symptoms as normal and only 5.69% aware about pelvic floor physiotherapy.
Conclusion
The study concludes that there is a high prevalence of PFDs and a substantial lack of knowledge and awareness regarding PFDs and its rehabilitation.
Keywords
pelvic floor disorders
pelvic floor rehabilitation
Australian Pelvic Floor Questionnaire
postpartum women
Introduction
Pelvic floor disorders (PFDs) refer to a constellation of symptoms and structural changes related to abnormal functioning of pelvic floor musculature. The dysfunction corresponds to either increased activity (hypertonicity), diminished activity (hypotonicity), or incoordination of the pelvic floor muscles.1 It is a crucial yet overlooked health care issue with pregnancy, childbirth, and menopause being the major risk factors.2 The integrity of internal organs is maintained by the appropriate coordination of pelvic floor with the nervous system, as well as the well-coordinated contraction and relaxation of pelvic floor muscles, which help with continence, micturition, defecation, sexual activity, and childbirth.3 Pregnancy brings tremendous hormonal and physical changes in the female body which is associated with increased muscle fatigue predisposing women to experiencing PFDs like bowel and bladder incontinence, flatus incontinence, voiding dysfunctions, constipation, sexual dysfunctions, pelvic pain, and pelvic organ prolapse (POP) in the postpartum period.3,4 Pelvic floor problems bring embarrassment to most women and are still a taboo, making them a neglected area of women's health and an important public health issue. The literature on prevalence of PFDs in postpartum females in Indian population is limited, wherein studies assessing all domains of pelvic health are scarce. Furthermore, no studies, in the Indian population, have concentrated on assessing the awareness of role of physiotherapy for the treatment of PFDs. Most females are reluctant to report symptoms either due to embarrassment, lack of awareness about treatment options, or misconception about the normal aging process. Women usually seek help when the symptoms get severe to an extent wherein it mandates a surgical intervention. Pelvic floor rehabilitation is an evidence-based, low-risk, and minimally invasive intervention that can aid in the prevention, treatment, and/or management of PFDs.5 Hence, the present study intended to assess the knowledge and awareness of PFDs and rehabilitation in postpartum women.
Material and Methods
Primary data was collected from a tertiary care hospital in Belagavi city, Karnataka, India. The present study was a cross-sectional study and was approved by the Institutional Ethical Committee (ethical clearance no. 821). The sample size calculation was based on expected prevalence from the former studies using the formula, n = Z2 p (q)/d2.
The derived sample size was 316 for which nonprobability sampling was used with a sample of convenience. The study screened 423 postpartum females in a span of 6 months, out of which 316 women were included based on the following inclusion criteria: age between 21 and 40 years, within 6 months postpartum, those who had undergone at least one normal delivery (with or without episiotomy) or lower segment caesarean section, and those willing to participate. The exclusion criteria were pregnant females, those who had undergone recent pelvic floor surgeries, those with PFDs secondary to orthopaedic or neurological issues, and those with acute illnesses. Informed consent was obtained from all participants prior to inclusion in the study and the procedure was explained to all. Demographic data was recorded, and participants were administered the Australian Pelvic Floor Questionnaire (APFQ)6 along with six selfdesigned questions to assess their knowledge and awareness of PFDs and physiotherapy treatment. APFQ is an interviewer-administered pelvic floor questionnaire that incorporates four domains: bladder function, bowel function, sexual function, and POP, severity, bothersomeness, and condition-specific quality of life. Aggregate scores are calculated individually for the bladder, bowel, POP, and sexual symptom categories. The resulting scores are divided by the total score for each domain and multiplied by 10, yielding a value between 0 and 10 for each of the four domains and a summative global pelvic floor dysfunction score of 40. A higher score indicates the existence of pelvic floor abnormalities, whereas a lower value indicates the existence of an efficient pelvic floor. It has a Cronbach's alpha value of 0.72 for bladder function domain, 0.82 for bowel function domain, 0.81 for sexual function domain, and 0.95 for the domain of POP. The statistical analysis was done using SPSS software version 26.
Results
A total of 316 women, who were within 6 months postpartum and between the age of 21 and 40 years, were included in the study and the prevalence of each domain along with the percentage of pelvic floor affected was evaluated using the APFQ scoring system. Apart from this, six other questions were asked to assess the perception of PFDs and awareness about its rehabilitation. Table 1 shows the demographic data collected from the females.
| Mean | Standard deviation | |
|---|---|---|
| Age | 29.08 | 5.85 |
| Height | 156.3 | 6.75 |
| Weight | 56.94 | 9.73 |
| BMI | 23.32 | 3.98 |
| Menarche age | 13.06 | 1.12 |
| Age at marriage | 20.70 | 3.38 |
| Age at first delivery | 22.58 | 3.48 |
| Parity | 1.91 | 0.87 |
| Vaginal delivery | 0.52 | 0.49 |
| C-section | 0.50 | 0.50 |
Abbreviations: BMI, body mass index; C-section, cesarean section.
Fig. 1 shows the prevalence of each domain of PFD along with the global affection of pelvic floor. Bladder component was affected in 54.11%, bowel in 26.8%, prolapse in 2.21%, and sexual function in 22% postpartum women with a global affection in 63.6% postpartum women. Fig. 2 shows the percentage of pelvic floor affected in postpartum women. The pelvic floor was affected in the range of 0 to 5% in 109, 5 to 10% in 44,10 to 15% in 25,15 to 20% in 13,20 to 25% in 5,25 to 30% 1, and 30 to 35% in 4 postpartum women.
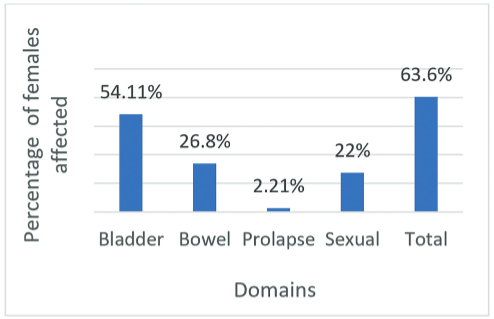
- Prevalence of pelvic floor disorders.
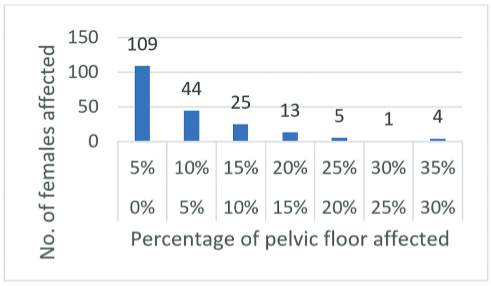
- Percentage of pelvic floor affected.
Based on the six questions asked to evaluate knowledge and perception, 84.4% women felt that the symptoms they were experiencing are normal whereas only 5.96% were aware about pelvic floor physiotherapy and that it can help alleviate these symptoms. None of these females had ever considered seeking any treatment, been assessed by a pelvic floor physiotherapist, or were aware about different treatment techniques in pelvic floor physiotherapy.
Out of the 316 females included in the study, 21 were illiterate, 134 had primary school education, 134 had high school education, 19 were graduates, and 8 were postgraduates.
Table 2 shows the correlation analysis, done between the level of education and the perception and awareness of PFDs and rehabilitation, and was found to be nonsignificant at 5% level of significance for awareness and effectiveness of pelvic floor rehabilitation and was significant at 5% level of significance for perception of PFDs.
| Serial no. | Correlation of level of education with | Coefficient of correlation (r) | p-Value |
|---|---|---|---|
| 1 | Perception of pelvic floor disorders | 0.1284 | 0.02* |
| 2 | Awareness of pelvic floor physiotherapy | 0.0174 | 0.75 |
| 3 | Effectiveness of pelvic floor physiotherapy | 0.0174 | 0.75 |
Discussion
PFDs are a significant impairment among women, especially after childbirth. The present study aimed to examine the knowledge and awareness of PFDs and rehabilitation among postpartum females.
The prevalence of PFDs in postpartum women has been studied in several regions of the world. The present study found the prevalence of PFDs to be 63.6% in women who were within 6 months postpartum between the age of 21 and 40 years. This is in agreement with research undertaken in South India among 26 villages of Tamil Nadu, which included all domains of pelvic health, namely, urinary incontinence (UI), fecal incontinence (FI), POP, sexual dysfunction, and pelvic pain, where the prevalence was found to be 54.7% in females between the age of 18 and 70 years.7
In India, a study done in Kuppam, found that 19.33% women visiting their gynecological outpatient department, suffered from some form of PFD which included POP, UI, or FI.8 Another study conducted in Udupi Taluk in Karnataka, reported a prevalence of 21% in married women with 19.02 and 1.99% suffering from UI and POP, respectively.9 In consonance with this, a study in North India reported a prevalence of 20.7% with inclusion of the domains of POP, UI, and FI along with flatus incontinence.10 The high prevalence rate from the present study can be attributed to the chosen study population (postpartum women) and the inclusion of the domain of sexual dysfunction which has not been addressed earlier along with UI, FI, and POP.
A longitudinal study by Hou and Tong in 2022, established the APFQ scores to be at the peak in the final trimester of pregnancy with a steady decline at 2 months, 6 months, and 3 years postpartum.11 Due to the hormonal and physical changes brought on by pregnancy, women are more susceptible to developing PFDs, namely, bowel and bladder incontinence, flatus incontinence, voiding dysfunctions, constipation, sexual dysfunctions, pelvic pain, and POP, during the postpartum period. Awider and anteriorly tilted pelvis, in addition to a gravid uterus, are physical abnormalities that might cause overstretching of the pelvic floor. The hormonal changes include the excessive secretion of relaxin and progesterone to make childbirth easier, which degrade elastin and modify collagen to relax the pelvic ligaments, muscles, and fascia, making the pelvic joints unstable and adversely affecting their supporting function.3,4,12–16
The female body requires around 6 weeks to 6 months to recover from these changes and even then, does not return back to its prepregnant state. This study also attempted to investigate and offer additional data on the influence of childbirth on pelvic floor dysfunctions. Hence, the age group of our study participants was between 21 and 40 years so as to eliminate the effect of hormonal fluctuations in the premenopausal age.
The Indian population has several cultural notions that restrict people from considering sexual function as a part of pelvic health. According to the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition criteria, fluctuations in gonadal hormone production, postpartum women are more susceptible to developing sexual dysfunctions such as hypo-active desire, painful sexual intercourse, arousal, and orgasmic disorder. It is typical to experience hypoactive sexual desire in the first 6 to 7 weeks after giving birth, but if it persists, it may strain relationships. Persistent dyspareunia and vaginismus, 60 to 180 days postpartum, may be caused by psychological, physical, or a combination of both. Culture also plays a vital role in this. Disorders related to arousal and orgasm frequently coexist with other illnesses.17,18
A study conducted in Tamil Nadu in 2019 is the only one in India apart from the present study to have included the domain of sexual dysfunction under the heading of pelvic floor dysfunctions, but as per our knowledge no other studies have particularly found the occurrence of sexual dysfunctions in postpartum females.7
The postpartum period offers the potential for prompt detection and management of pelvic floor problems. Despite the fact that postpartum pelvic floor abnormalities are common, the pelvic floor is not frequently examined in the context of health care. Questionnaires are adept in measuring these frequently qualitative symptoms, which usually remain unreported and might precipitate to comorbid conditions.19 To address this issue, eclectic rehabilitation techniques and interventions have been developed, but their usage is at a bare minimum. Hence, the present study highlights the importance of assessing the perception of PFDs and understanding of pelvic floor rehabilitation in postpartum women. It was found that 84.4% women in the present research believed that the symptoms they were experiencing were natural repercussions of pregnancy and childbirth and there was no need for them to be reported or treated. A mere 5.96% of these women were aware about pelvic floor physiotherapy and even they never considered seeking any treatment.
According to Snyder et al, lack of knowledge, time, and resources are the largest barriers for seeking pelvic health care. Women have an adverse mindset concerning their own pelvic health, with a general sense of self-care being a low priority.3 As a result, despite the frequent occurrence of pelvic floor issues, only a limited number of women seek medical attention, assistance, or guidance.
The present study also found that there was no correlation between level of education and awareness of pelvic floor physiotherapy which suggests that it is imperative to create awareness regarding PFDs and rehabilitation irrespective of the academic qualifications of women. By improving awareness, education, and access to resources, health care professionals can empower women to make informed decisions about their pelvic floor health.
The present research is limited by its single-center design and brief duration. Nevertheless, it is innovative in its examination of perception of PFDs, awareness of pelvic floor physiotherapy, and comprehensive evaluation of various aspects of pelvic floor function.
Conclusion
According to the findings of the current study, the prevalence of PFDs is 63.6% and there is a substantial lack of knowledge and awareness regarding PFDs and its rehabilitation with only5.96% women being aware about it and 84.4% women considering the symptoms normal. It emphasizes the need for comprehensive education and antenatal-postnatal care programs to improve pelvic floor knowledge and prevent long-term complications. Further research and targeted interventions are necessary to bridge the knowledge gaps and promote optimal pelvic floor health among postpartum women.
Conflict of Interest
None declared.
References
- Pelvic Floor Dysfunction In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2022. In:
- [Google Scholar]
- Knowledge of the pelvic floor in menopausal women and in peripartum women. J Phys Ther Sci. 2016;28(11):3020-3029.
- [Google Scholar]
- “We don't talk about it enough”: perceptions of pelvic health among postpartum women in rural communities. Womens Health (Lond Engl). 2022;18:17455057221122584.
- [Google Scholar]
- The most common functional disorders and factors affecting female pelvic floor. Life (Basel). 2021;11(12):1397.
- [Google Scholar]
- Pelvic floor physical therapy in the treatment of pelvic floor dysfunction in women. Curr Opin Obstet Gynecol. 2019;31(06):485-493.
- [Google Scholar]
- An interviewer-administered validated female pelvic floor questionnaire for community-based research. Menopause. 2008;15(05):973-977.
- [Google Scholar]
- Prevalence of pelvic floor dysfunction among women inSouth India. Int J Nurs Educ. 2019;11(04):171-175.
- [Google Scholar]
- Prevalence of pelvic floor dysfunction in women attending obstetrics and gynaecology OPD at PES Institute of Medical Sciences and Research, Kuppam. Int J Reprod Contracept Obstet Gynecol. 2020;9(12):5087-5094.
- [Google Scholar]
- Prevalence of pelvic floor dysfunction among married women of Udupi Taluk, Karnataka, India. J Womens Health Care. 2015;4(03):x.
- [Google Scholar]
- Prevalence of pelvic floor dysfunction in postpartum women. Indian Obstet Gynaecol. 2020;10(02):13-17.
- [Google Scholar]
- Three-year follow-up of a self-administered Australian pelvic floor questionnaire validated in Chinese pregnant and postpartum women. Int Urogynecol J. 2022;33(11):3077-3084.
- [Google Scholar]
- Impact of subsequent pregnancies on pelvic floor functional anatomy. Int Urogynecol J. 2018;29(10):1517-1522.
- [Google Scholar]
- Elastin metabolism in pelvic tissues: is it modulated by reproductive hormones? Am J Obstet Gynecol. 2005;192(05):1605-1613.
- [Google Scholar]
- A review of the epidemiology and pathophysiology of pelvic floor dysfunction: do racial differences matter? J Obstet Gynaecol Can. 2005;27(03):251-259.
- [Google Scholar]
- The effect of relaxin on the musculoskeletal system. Scand J Med Sci Sports. 2014;24(04):e220-e229.
- [Google Scholar]
- Pelvic alignment changes during the perinatal period. Plos One. 2019;14(10):e0223776.
- [Google Scholar]
- Postpartum female sexual function: risk factors for postpartum sexual dysfunction. Sex Med. 2020;8(01):8-13.
- [Google Scholar]
- Postpartum sexual dysfunction: a literature review of risk factors and role of mode of delivery. BJMP. 2010;3:316-320.
- [Google Scholar]
- Questionnaires to evaluate pelvic floor dysfunction in the postpartum period: a systematic review. Int J Womens Health. 2018;10:409-424.
- [Google Scholar]