Translate this page into:
A Case Report of Citelli’s Abscess: A Rare Complication of Mastoid Abscess
Address for correspondence Ayushi Sharma, MBBS, MS, Department of ENT, NITTE (Deemed to be University), K. S. Hegde Medical Academy, Mangalore 575018, Karnataka, India (e-mail: ayushisharma9092@gmail.com).
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Middle ear and the tympanic membrane are complex structures. Anatomy is destroyed in cases with extensive inflammation. It is better to avoid middle ear surgical intervention in such cases until the inflammation subsides. Here, we present a 70- year-old immunocompromised male, who presented with foul-smelling discharge from the right ear and a painful swelling over right side of the neck, diagnosed as a case of coalescent mastoiditis with abscess along the digastric muscle. Patient was successfully managed with initial incision and drainage of the abscesses and intravenous antibiotics without manipulating the middle ear and external auditory canal.
Keywords
mastoid abscess
surgery
middle ear surgery
Background
Acute mastoiditis leading to deep neck abscesses like Citelli’s abscess and Bezold’s abscess has become very rare in the present antibiotic era.1 When the pus from the mastoid tip drains down along the posterior belly of the digastric muscle to the occipital and cervical region, it is known as Citelli’s abscess.2
In immunocompromised conditions like diabetes mellitus and human immunodeficiency virus/acquired immune deficiency syndrome, patients are more prone to atypical complications like deep neck space infections.3 Timely recognition has a key role in the management and in case of any delay, there are high chances of airway obstruction and mediastinitis due to descending infection.4
These are rare complications of otologic origin. As initial manifestations appear to be nonthreatening, it can lead to a delay in diagnosis. High level of clinical suspicion and the early use of imaging can avoid dreaded complications in these patients.5 Early broad-spectrum antibiotics and management of diabetes and other immunocompromised conditions can prevent complications. Culture and sensitivity testing of the ear discharge and treatment with appropriate antibiotics play a major role in the timely management of these cases.6 Cases with diagnoses of multiple abscesses may involve multiple causative organisms, thereby requiring separate culture and sensitivity testing of pus drained from each site.
Case Presentation
A 70-year-old male, a known case of type II diabetes mellitus, systemic hypertension, and dilated cardiomyopathy on medications, presented with complaints of foul-smelling discharge from the right ear since 1 month along with dysphagia and pain in the upper part of right side of the neck since 1 week.
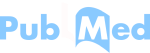
On examination, purulent discharge was noted in the right ear canal along with granulation tissue in the floor of the external auditory canal and tenderness in the right mastoid area. The right tympanic membrane was not visualized clearly because of ear canal wall edema (Fig. 1A).
- (a) right external auditory canal wall edema and granulation tissue; (b) * shows swelling in the right submandibular region which patient had presented with.
Bilateral tonsils, posterior pillars, and posterior pharyngeal wall were congested. On video laryngoscopy, a bulge was noted in the posterior pharyngeal wall along with inflammation of aryepiglottic folds. A tender and diffuse swelling was noted over the right side of the neck below the mandible (Fig. 1B).
A provisional diagnosis of right chronic otitis media with Ludwig’s angina was made. Patient was immediately put on intravenous antibiotics, after which there was improvement in dysphagia and oropharyngeal and hypopharyngeal edema subsided.
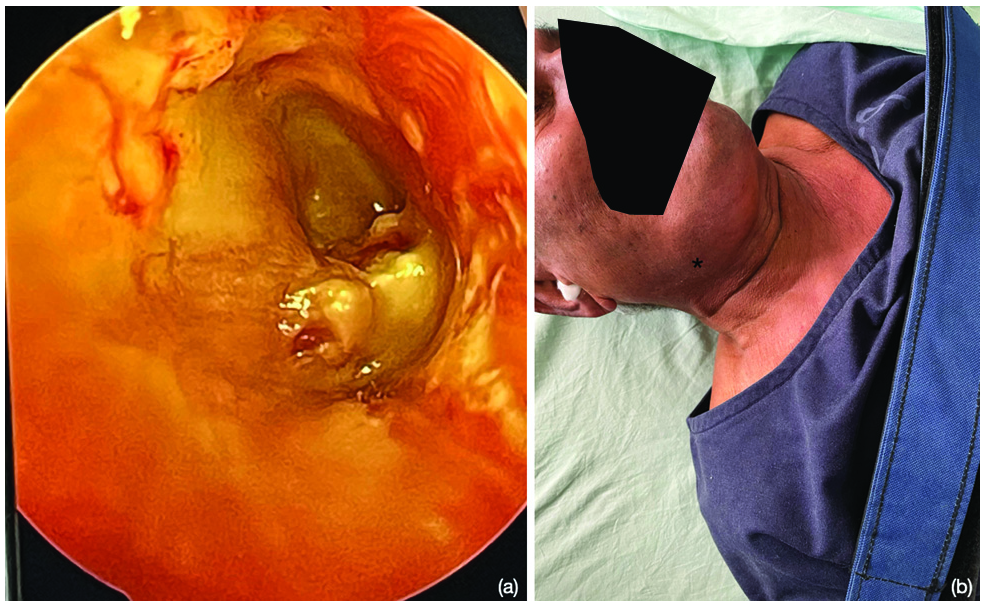
Contrast-enhanced computed tomography showed right mastoid abscess extending to posterior and anterior bellies of right digastric muscles. Diffuse inflammation of structures of right side of neck and pharynx was noted. There was nonenhancing hyper-density in the right mastoid with obliteration of mastoid air cells. Inferomedially, there was erosion of mastoid wall and extension of content into the posterior belly of digastric muscle, which appeared thickened with heterogenous enhancement (Fig. 2A, B).
- (a) CECT head axial section * showing obliteration of right mastoid air cells; (b) CECT head coronal section * showing mastoid abscess extension into right digastric muscle.
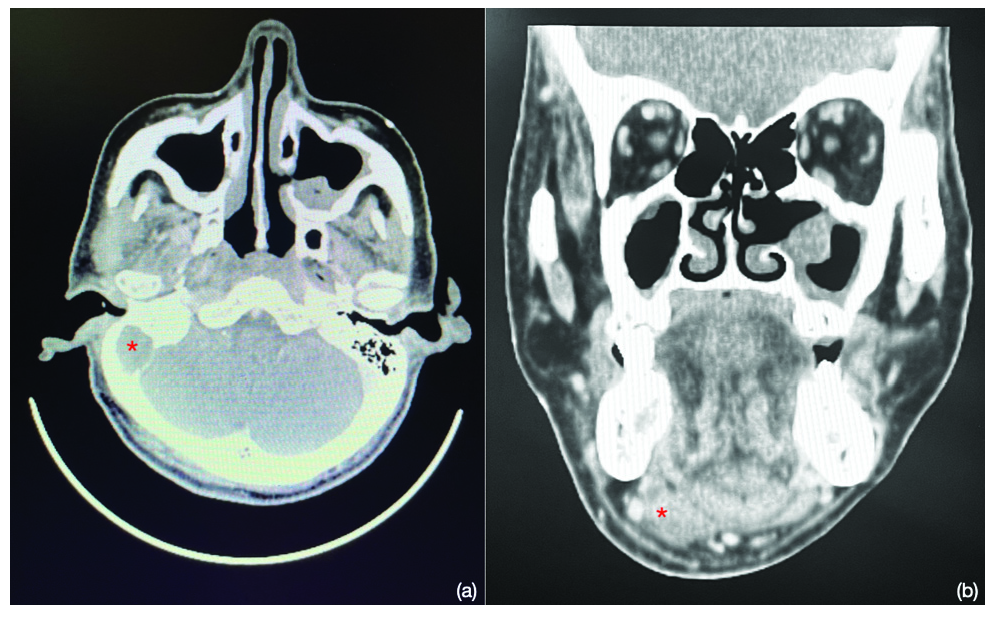
In magnetic resonance imaging, there was peripheral enhancing collection within the right mastoid with erosion of medial cortex and extending into the right digastric muscle—suggestive of mastoid abscess with extension to the floor of mouth. Bony erosions of the skull base with focal enhancing thickening of the adjacent pachymeninges were noted, which was suggestive of meningitis (Fig. 3).
- MRI head axial section. * showing right digastric muscle abscess.
A diagnosis of right coalescent mastoiditis with extension into the posterior belly of right digastric muscle was made. Patient was immediately started on intravenous antibiotics. Mastoid abscess was drained by postaural incision and removing the outer cortical bone (Fig. 4).
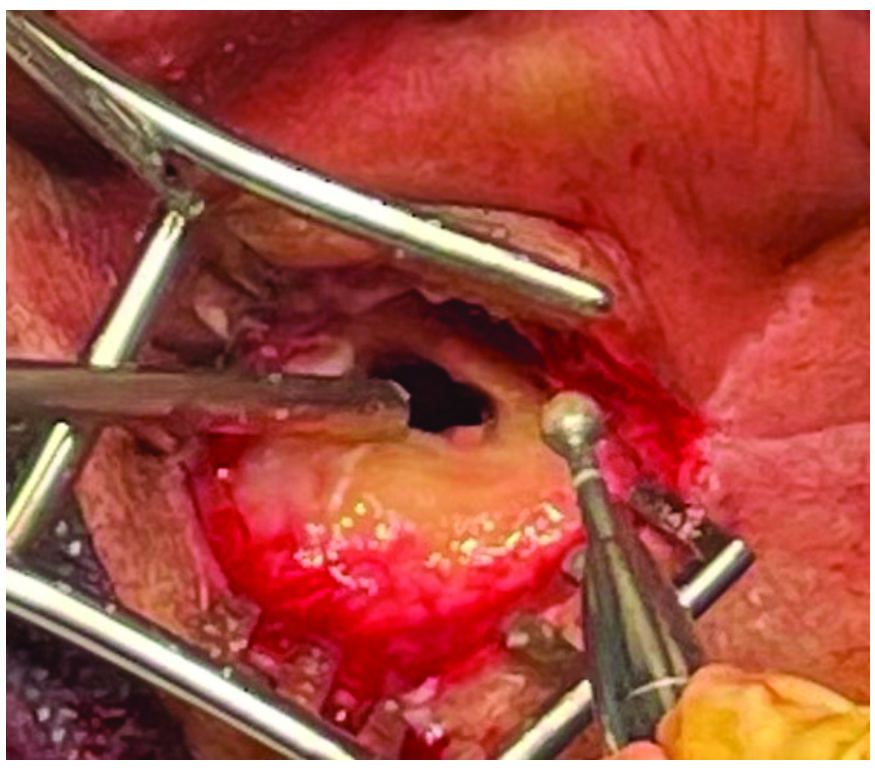
- Intraoperative picture of right mastoid abscess drainage by postaural incision and cortical mastoidectomy.
A 4 cm transverse incision was made 2 cm below the right angle of mandible, the neck abscess was traced along the posterior belly of right digastric muscle, and 15 mL pus was drained.
As canal wall was severely oedematous and the normal landmarks were lost, the middle ear inspection was planned in a staged manner and the patient was convinced regarding the need for further surgery.
Pus drained from both the neck abscess and the mastoid cavity was sent for culture and sensitivity testing. The right ear swab and pus from mastoid abscess showed growth of methicillin-resistant Staphylococcus aureus, whereas pus from the neck abscess showed growth of Klebsiella pneumoniae. Both the organisms were sensitive only to Linezolid. The patient was treated with intravenous Linezolid 600 mg, twice a day for 7 days. On the third postoperative day, we could visualize the tympanic membrane on otoendoscopy. The right ear canal and the tympanic membrane were nearly normal after 1 month of follow-up with minimum conductive hearing loss.
Discussion
Presence of external auditory canal infection is a relative contraindication for tympanoplasty and middle ear reconstructive surgeries in our clinical practice. There are hardly any articles regarding the standard criteria for status of ear canal skin in tympanoplasties and middle ear surgeries. We could find only one article regarding otomycosis of external auditory canal in tympanoplasty.7 For middle ear surgery, canal skin plays a crucial role. The presence of canal wall inflammation may affect the tympanomeatal flap elevation in middle ear surgeries.
In the presence of extensive edema of the ear canal, the visualization of middle ear structures is difficult. Once the infection is under control, the normal landmarks will be clear. In this case, we avoided canal wall manipulation while draining the mastoid abscess as it was difficult to find the normal anatomical landmarks. Following treatment with abscess drainage and intravenous antibiotics, the ear canal and middle ear inflammation also subsided. We would like to highlight here that extensive surgeries should be avoided when landmarks are not clear, and can be done as a staged procedure.
Both gram-positive and gram-negative organisms are known to cause middle ear infections. The common organisms are S. aureus, Pseudomonas, Escherichia coli, Klebsiella, etc. Linezolid and vancomycin are highly sensitive against Staphylococcus. Amoxicillin followed by doxycycline, amikacin, and levofloxacin are the other sensitive drugs. Gram- negative organisms like Pseudomonas and Klebsiella are sensitive to meropenem and amikacin.8
The most commonly isolated organisms in head and neck abscesses are S. aureus and Bacteroides species.9 In deep neck space infection, the bacteriology is usually polymicrobial, including both aerobic and anaerobic bacteria. Streptococcus pyogenes and S. aureus are the most common aerobic bacteria, whereas Peptostreptococcus species, Prevotella species, Propionibacterium species, and Fusobacterium species are the most common anaerobic bacteria.10 The most common bacteria in diabetic patients is Klebsiella pneumoniae.11
In our patient, the organisms were different in the two abscesses even though the neck abscess had originated from the mastoid abscess itself. So, we would also like to highlight here that whenever abscesses are drained at multiple sites, even if the origins are the same, drained pus from each site should be sent for culture and sensitivity testing separately. Here, although both organisms were different, both were sensitive to Linezolid.
Citelli’s abscess occurs either due to direct extension from mastoid tip area through fascial or subcutaneous plane or mastoid emissary vein. Radiological imaging is mandatory prior to incision and drainage to rule out associated complications. Drainage of pus will relieve pain, hence improving the patient’s condition and it will inhibit further spread to the intracranial cavity.
Conclusion
Surgical manipulation of the middle ear or external auditory canal wall should be avoided in such cases with severe canal wall edema or inflammation. In cases with multiple abscesses or multiple sites of pus collection, the drained pus should be sent for culture and sensitivity testing separately for each site as the microorganisms involved can be different for each site. This will help in providing appropriate antibiotic coverage for the respective causative organisms.
Conflict of Interest
Nil.
References
- Citelli’s abscess following otitis media: a case report. Iran J Otorhinolaryngol. 2017;29(92):161-163.
- [Google Scholar]
- Importance of early identification of a deep neck abscess [in Dutch] Ned Tijdschr Tandheelkd. 2022;129(04):175-183.
- [Google Scholar]
- Deep neck space infections: current trends and intricacies of management? Indian J Otolaryngol Head Neck Surg. 2022;74(Suppl 2):2344-2349.
- [Google Scholar]
- Treatment of otomycosis in ears with tympanic membrane perforation is easier with paper patch. Turk Arch Otorhinolaryngol. 2019;57(04):182-186.
- [Google Scholar]
- Microbiology of chronic otitis media and shifting trends of its antibiotic susceptibility: a prospective observational study in a tertiary care institute of Western Rajasthan. Indian J Otolaryngol Head Neck Surg. 2022;74(Suppl 3):3748-3753.
- [Google Scholar]
- Diagnosis and management of anaerobic infections of the head and neck. Ann Otol Rhinol Laryngol Suppl. 1992;155:9-15.
- [Google Scholar]
- Bacteriology of deep neck infections: analysis of 634 patients. Aust Dent J. 2015;60(02):212-215.
- [Google Scholar]
- Bacteriology of deep neck abscesses: a retrospective review of 96 consecutive cases. Singapore Med J. 2011;52(05):351-355.
- [Google Scholar]